Trauma Informed Care in Primary Health Settings
Dr Jasmine Pang describes the impact early adverse childhood experiences have on individual later-life health and well-being, with advice for general practitioners and health providers in how to provide trauma-informed care.
Primary health settings provide a unique environment for the provision of trauma informed care. Many trauma survivors do not seek mental health services but look for help in primary care settings. Neither patient nor providers may be aware of the link between their current physical complaints and the connection to past trauma. Yet research has clearly shown a wide-ranging impact of Adverse Childhood Experiences (ACE).
The CDC-Kaiser Permanente Adverse Childhood Experiences (ACE) Study is one of the largest investigations of childhood abuse and neglect and the links to later-life health and well-being. ACEs investigated included emotional abuse, physical abuse, sexual abuse, household intimate partner violence, household substance abuse, household mental illness, parental separation or divorce and incarcerated household members.
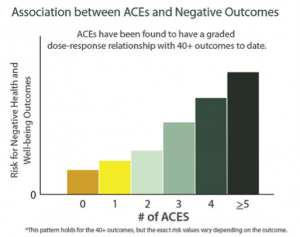
Results of the study found that almost two thirds of study participants reported at least one ACE, and more than one in five reported three or more ACEs. The study also found a graded dose response relationship between ACEs and negative health and well being outcomes across the life course.
The study showed that as the number of ACEs increases so does the risk for the following-
- Depression
- Fetal death
- Health-related quality of life
- Illicit drug use
- Ischemic heart disease
- Liver disease
- Poor work performance
- Financial stress
- Risk for intimate partner violence
- Multiple sexual partners
- Sexually transmitted diseases
- Smoking
- Suicide attempts
- Unintended pregnancies
- Early initiation of smoking
- Early initiation of sexual activity
- Adolescent pregnancy
- Risk for sexual violence
- Poor academic achievement
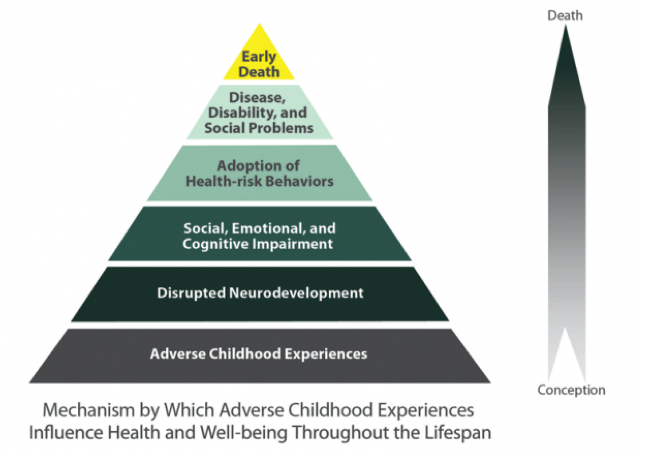
ACEs continue to have a lifelong impact from conception to death as it disrupts neurodevelopment. This results in social, emotional and cognitive impairment, which causes the adoption of high health risk behaviours leading to disease, disability and social problems.
Role of General Practitioners
Despite the increasing evidence of the lifelong health impact of ACEs, research shows that less than one-third of primary care doctors screen for ACEs on a regular basis [1]. This was often due to a lack of knowledge of the prevalence of ACEs, discomfort with asking screening questions and perceived role. Yet, the primary care physician is uniquely positioned to play a critical role in the identification of ACEs and facilitating appropriate treatment. Interacting with adults, children and their families at regular intervals can allow patients and providers to develop a trusting relationship, which can facilitate the disclosure of ACEs. Contrary to popular belief, research has shown that screening for adversity is acceptable amongst patients. In an adult primary care setting, 79% of patients were comfortable being asked about ACEs and 86% felt comfortable being screened for ACEs[2]. However, patients would only disclose if asked directly in a safe supportive manner. In a study at the Health Appraisal Clinic at Kaiser Permanente of San Diego, there was a 35% decrease in office visits and an 11% decrease in emergency room visits among participants compared to the prior year[3] when they started screening for ACEs. Addressing childhood adversity in medical settings offers clinicians a more complete picture of important social determinants of health and has a great potential to improve health care utilization and encourage help seeking behavior.
What is trauma informed care?
A programme, organization or system that is trauma informed realizes the widespread impact of trauma and understands potential paths for healing; recognizes the signs and symptoms of trauma in staff, clients and others involved with the system; and responds by fully integrating knowledge about trauma into policies, procedures, practices and settings.
What can General Practitioners do?
- Learn more about the provision of trauma informed care and about trauma. Understand that “problem behaviours” may be manifestations or symptoms of trauma, or coping skills that served to protect them when surviving their trauma.
- Routinely ask patients about trauma history and trauma symptoms. This can be done using formal screening tools (E.g. Primary Care PTSD Screen, Brief Trauma Questionnaire) or by asking if patients had ever experienced one of the 10 ACEs identified in the ACEs study. Find out more about how to do so in a way that patients can feel supported to disclose.
- Discuss the impact of identified traumatic events if the patient screens positive. Not everybody who has experienced ACEs have ongoing difficulties. It is important to explore if current functioning has been impacted and the patient continues to experience distress from the traumatic experience
- Provide a referral if needed
- Follow up with the patient
[1] Weinreb, L., et al (2010) Primary Care Companion Journal of Clinical Psychiatry, Screening of trauma in adult primary care settings, 12(6)
[2] Goldstein, E., Athale, N., Sciolla, A. F., & Catz, S. L. (2017). Patient Preferences for Discussing Childhood Trauma in Primary Care. The Permanente Journal, 21.
[3] Felitti, V. J., & Anda, R. F. (2014). The lifelong effects of adverse childhood experiences. Chadwick’s child maltreatment: sexual abuse and psychological maltreatment, 2, 203-15.
 This article was written by Dr Jasmine Pang at Benchmark Psychology. Jasmine has a particular interest in supporting children, adolescents, parents and adults who have experienced traumatic or difficult life circumstances and is passionate about ensuring high quality services be made available to them.
This article was written by Dr Jasmine Pang at Benchmark Psychology. Jasmine has a particular interest in supporting children, adolescents, parents and adults who have experienced traumatic or difficult life circumstances and is passionate about ensuring high quality services be made available to them.